Life and Wellness Blog
Day 20: How to Engage in Effective Distractions
🎉Seek distractions to move through distress. Hobbies, contributions, opposite emotions,👏other...
Breaking Free from the Comparison Trap: Crafting Your Uniquely Empowered Life
In a world where societal expectations often shape our ideals...
Day 19: You Must Be Able To Control Your Moments Especially in Times of Distress
👉Tolerate and accept distress. 🔎Identify effective strategies to 🚧navigate through...
Embracing Me-Time: The Transformative Power of Prioritizing Self-Care
Setting aside time for yourself is crucial for maintaining overall...
Day 18: The Secret About What’s the Resolution
👀Focus on the problem, not the person.🤠 Resolve ⚡conflicts by...
Day 17: Hear What People Are Really Saying
👏Improve communication through active 👂listening. Pay attention,📌acknowledge, and provide 🗣feedback....
Day 16: Observe How You Really Handle Yourself and Your Situations
⚡Observe your responses – passive, aggressive, or assertive. ⚡ 🔎Enhance...
Seizing the Moment: A Journey to Recovery from Alcohol Addiction
In the tapestry of life, every thread represents an opportunity...
Day 15: Tactics of Assertiveness Do You Have Them?
⚡Develop the skill of assertiveness 👈👉 a balanced response. 🦸♂️Stand...
Day 14: Time to Get Effective and Do What Works – Are You Mindful and Willing?
😵💫”Focusing on what is 🔎present, embrace🫂 effectiveness over ⬆️right versus...
Day 13: Limits and Limitations at Their Finest – They Don’t Make Them Like They Used To!
➡️Set limits and⚖️limitations to stay within your💪strengths.⬅️ ➡️Establish boundaries🤔with assertiveness...
Day 12: Mastering Boundaries: Create Your Filtrating System for Ultimate Empowerment
💥Empowerment👀 Join us on a journey🗼of self-discovery😊as we delve into...
Day 11: The Ripple Effect of Kindness
Kindness is a ripple that transforms lives. Extend kindness to...
Day 10: Mindful Eating for Holistic Health
Savor the flavors of🧠mindful🍎eating. Nourish not just your🚶♀️body but your...
Day 9: Navigate Through Negative Self-Talk
💪 Conquer negative self-talk.🗣 Rewrite 🖊 your inner narrative with...
Day 8: Redefine Your Relationship With Time
⏰Time is a precious resource. Redefine your ⏳relationship with it....
Day 5: The Mirror Of Self-Reflection
👀Look into the🪞 mirror of self-reflection. Acknowledge your 🚴journey, confront your...
Day 3: Turn Those Beliefs That ‘Cost’ You into ‘Benefits’ That Reward You.
👉 Turn Those Beliefs That ‘Cost’ You into ‘Benefits’ That...
Day 2: Embrace Your Inner Voice
Believe in the transformative power within you. Embrace your inner...
Day 1: It’s Not Just About Rating Your Health
Understand how sobriety, emotional wellbeing, and holistic health intersect in...
Ignite Your Soul: The Transformative Power of Embracing Dry January
As we approach the threshold of a new year, many...
A New Chapter: Embracing Sobriety in 2024 with Turning Leaves Recovery
As we stand on the start of a brand new...
Navigating Sobriety with Confidence: Tip #6 – Celebrating Sobriety During the Holidays 🌟
As the holiday season approaches, we delve into Tip #6...
Crafting Joyful Sobriety: Navigating Sobriety with Confidence Tip #5
As we approach the holiday season, Tip #5 in our...
Navigating Sobriety with Confidence: Tip #4 – Embracing Sobriety During the Holidays
As we immerse ourselves in the holiday season, individuals on...
Navigating Sobriety with Confidence: Tip #3 – Mindful Sobriety 🌿
“Navigating Sobriety with Confidence,” we delve into Tip #3: Mindful...
Navigating Sobriety with Confidence: Tip #2 – Planning Ahead for Social Gatherings 🌟
Embarking on the journey of sobriety during the holiday season...
Top 6 Tips of Sobriety – Tip #1 Surround Yourself with a supportive Network
Surround yourself with a supportive network of friends, family, or...
Understanding and Managing Intrusive Thoughts: A Journey to Mental Wellness
Today, let’s delve into the realm of intrusive thoughts—those unwelcome...
🌱 Exploring Healthy Living: Investigating Our Fueling Practices! 🍏🧠
👋 Join me on an incredible journey of nourishing our...
🌿 Embrace the Power of a Healthy Daily Routine! 🌞
👋 Today, let’s dive into the transformative magic that unfolds...
Living a Truly Recovered Life: Choosing It, Owning It, Living It
Introduction: Recovery is not just about overcoming challenges; it’s about...
Do You know how to instigate Frustration Tolerance?
We all need to create the capacity to endure this...
Know your challenge and approach with calmness
“People become inspired and expansive when they pull together to...
You, Unstuck, Enjoying Your World, The People in it, Just the Way You Dream About It!
You, Unstuck, Enjoying Your World, The People in it, Just...
Are you afraid to go back to what we thought was normal?
Do you feel in control? Are you afraid to go...
Life Continues To Unfold – How are You Responding?
Life continues to unfold – How are you responding? Hey...
Operation Objective Self-Observation: Part 2
“But when we observe, we are forced to pay attention....
DON’T BE HELD HOSTAGE BY YOUR HABITS: 10 STEPS TO LIVE FREE AND STAY THERE
Do you ever feel like you’re being tied down to...
How to Cultivate Your Confidence & Say How You Feel!
Why is the articulation of our feelings such a challenge?...
A CLOSING THANK YOU: THE GRATITUDE WE LEAD WITHIN OUR FAMILIES
As a closing Thank You, I think It’s time to...
How will you get there? | Knowing where or how you want to be won’t make it happen… Action will!
I have been in a lot of “places” in my...
The Narrow Perspective Around Addiction – It’s Remarkable.
Let me ask you something. Have you ever hidden an...
You are capable of amazing things! 6 steps to an Intentional Life Recovery Journey
It is possible to live free from addictions, negative attachments,...
WHAT DO YOU SEE? HOW TO EFFECTIVELY FACE AND CONTROL YOUR EMOTIONS
What do you see in the mirror? A victim, someone...
HOW TO OVERCOME PRESSURES AND PANDEMICS WITH PURPOSEFUL PLANNING
Wow! Hello everyone, just shy of being one week away...
Living In My Intuition
in·tu·i·tion /ˌint(y)o͞oˈiSH(ə)n/ noun 1. the ability to understand something immediately,...
My Journey, Your Success: Celebrating 8 Years of Freedom!
The longer I have been sober the more I realize...
Positive, Productive, Passionate: My 3 Truths To Living In Recovery!
Before you read any further, I want to give you...
You Are Pretty & Special | A Conversation About Body Image
What does it sound like inside when you think about...
Are You A What If’er? | Let’s talk about how to keep this dialog motivating instead of stifling.
You know who you are. Right? You are the one...
Life Transitions Can Get Tricky | Shifting into an intuitive mindset will change your experience.
Life transitions can get tricky. They insight feelings that we...
Perceptions are funny things | A thought provoking discussion that just may change yours.
Isn’t it interesting how what one person experiences as tragic...
Hey Mom’s, I Hear You Need To Find Alone Time! | Let’s Talk About Why This Is A Challenge
I want to start by saying I am in no...
What Example Am I REALLY Leading By | A look at how the way you operate is affecting you and others!
Look, here’s the deal. Regardless of what your role is...
Stop wasting your time worrying about what others think about you!
Are you seemingly frozen in time? Feeling paralyzed in your...
Stop making excuses | Get busy figuring out what freezes you.
If you fell and broke your leg what would you...
Beginning the Recovery Process? Ask Yourself These 5 Questions and Break the “Habit” Cycle
Julie-Anne Tucker TLR Affiliate Coach November 18, 2021 How do...
Learn How to Give to Yourself and Others | 6 Effective Steps to Shift your Mindset.
I want to be pretty to the point this week....
Dry January, Sober Consciousness? Is it for you?
I want to take you through a very special journey,...
You Choose Your Actions! | Have you thought about why you make the ones you do?
You choose your actions! This is a fair statement, right?...
The roadmap to Intuitive thinking: The 10 things you need on your life recovery journey!
Creating an improved state of mental clarity requires a conscious...
The Colossal Decisions | Committing, where we fall short, and why we don’t have to!
When was the last time you decided without any hesitancy...
You CAN’T Spell Challenge Without Change. 3 tips you can’t skip!
You CAN’T Spell Challenge Without Change | Tricia Parido Master...
Oh, The Thanksgiving Stuffingness | One way you can have all the pleasure without the pain!
Oh Thanksgiving! For any of you out there that know...
Choice Overload! Is it the source of your anxiety and uncertainty?
Jordan Wright | TLR Affiliate | BS Psych October 22,...
Holiday Hurt Feelings? | What to do after the gathering when your ego is bruised!
Well, if you celebrated the Thanksgiving holiday, how did it...
What Assertiveness Is and is NOT
JULIE-ANNE TUCKER | AFFILIATE COACH | February 2, 2022 Communication...
Leaving It All Behind | No more negative attachments? That’s right. It can be done!
Everybody has something that they are attached to that impacts...
8 Steps to Uncover Why The Change We Seek Is Not The Change We Desire. It is a byproduct.
I guarantee you that what you are putting on the...
Sick and tired of being sick, tired, AND emotionally challenged? 5 steps to reducing vulnerability
Reducing vulnerability isn’t rocket science but does take work! Let’s...
Service Providers: How to Maintain Sound Mind and Emotional Intelligence
Service providers have a unique opportunity to impact the lives...
It’s Summertime! A Message for Early Recovery
Summertime brings up and out a lot of different things...
Barriers & Distractions we face and How to Overcome Them
There are countless barriers and distractions that can stand in...
How to find your Why and start living on your own terms
Have you ever felt dismissed or unheard, or like your...
Self Validation – A Better YOU, A Better Tomorrow
Self-validation is one of the most important things we can...
Overindulging During the Holidays
Did you find yourself overindulging in drinking this past Holiday...
The Epidemic of Stress in America: How People Are Coping
It is no secret that Americans are struggling with stress....
Don’t Let the Seasonal Stress Get the Best of You
We’re rolling into the Holiday Season! The holidays are a...
Bouncing Back Stronger: Overcoming Relapse
Relapse is a common and often challenging experience faced by...
You are capable of amazing things! 6 steps to an Intentional Life Recovery Journey
It is possible to live free from addictions, negative attachments,...
Actively Healing in Recovery
Written By: Katherine Polychron TLR Coaching Affiliate Are you feeling...
Remaining Sober Conscious at Festive Events!
Big events, whether they be holidays or weddings, are generally...
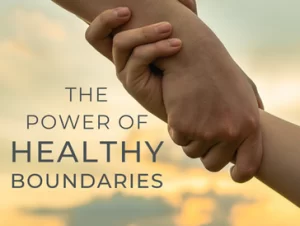
The Power of Placing Healthy Boundaries
Healthy relationships are built on respect, trust, and understanding. Therefore,...
How We Understand the Changes in Our Life
If you’ve ever found yourself feeling overwhelmed by the changes...
How to Create an Aspirational Plan and Focus on the Now
Do you find yourself feeling anxious and overwhelmed when trying...
Coaching = Effective Psychological Practice
Coaching has been researched and proven to be an effective...
Just because something is hard, it doesn’t mean it can’t be done.
Coach Mari Sullivan | Limiting Belief Specialist I see you....
What you were programmed to believe you could do
Published by Coach Mari Sullivan February 8, 2023 Even in...
Shaking Things Up: Why It’s Time for a Change When Life Seems Stuck in Neutral!
“Do stuff. Be clenched, curious. Not waiting for inspiration’s shove...
Mastering Your Day: 5 Steps to Take Control of Your Mindset and Transform Your Life
Are you tired of constantly putting others’ needs before your...
Unleashing Resilience: Navigating Crisis with Confidence and Courage!
1. Release negativity: Take a moment to write down all...
Freedom from Substance: Empowering Lives through Life Recovery Coaching
Breaking free from the clutches of substance use is a...
Unmasking ED: Navigating the Twists and Turns of Eating Disorder Recovery
Describing an eating disorder to someone who has never experienced...
Unlocking the Power of Family
A Healing Journey for Successful Women Breaking Free from Perfectionism...
Unleashing Your True Potential
Breaking Free from Destructive Coping Habits In today’s fast-paced world,...
Is Your Teen Using Drugs? A Parent’s Guide to Understanding and Support
Recognizing the Signs: Indicators That Might Warrant Your Attention Professional...
Embracing Relief Beyond Quick Fixes: Finding Calm Amid Overwhelm
In the whirlwind of life, moments of overwhelm can seem...
Celebrating Recovery Month: Your Journey to Sobriety and Healing
Welcome to Recovery Month, a time dedicated to recognizing the...
Embrace Gratitude for Personal Peace and Overcoming Emotional Challenges
In a world filled with emotional struggles, overwhelming perfectionism, negative...
Unlocking Financial Freedom: Marketing for Recovery
Recovery from addiction is a challenging journey that often demands...
Unlocking the Truth: Alcohol Consumption and Women’s Health (Ages 35-65)
When it comes to women’s health, it’s essential to explore...